OSTEOSARCOMA DE FEMUR
OSTEOSARCOMA OF FEMUR
INTRODUCTION:
Osteosarcoma is a mesenquimal neoplasm in which the tumor cells produce bone. Is the most common primary malignant solid tumor of bone because plasma
cell myeloma is actually the most common primary bone tumor but it's not
a solid tumor. (Cancer Treat Res 2009;152:3). We report a case of osteosarcoma of bone in a young lady that had a long history of pain on her left knee.

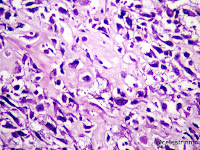
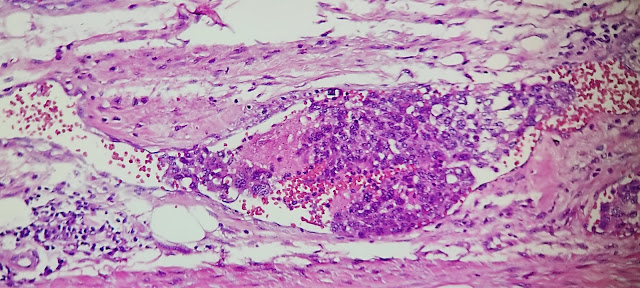
MICROSCOPIC IMAGES:
sheets of atypical large, epithelial-like cells.
Eosinophylic osteoid formation between the tumour cells.
Osteoid formation with calcification.
prominent vascular invasion.
Epitheliod-like tumour cells.
FOCAL chondroblastic differentiation.
BIBLIOGRAFY REVIEW:
Epidemiology 💹:
📌Incidence: most common high grade sarcoma of skeleton
📌Age (bimodal age distribution): (Cancer Treat Res 2009;152:3) (Cancer 2009;115:1531)
- Most cases: 10 - 14 year old
- Second smaller peak: adults (> 40 year old) - usually secondary osteosarcoma.
📌Paget disease of bone: ~ 1% (variable range among studies) of patients develop conventional osteosarcoma (55 - 70% arises in polyostotic Paget disease) (Bone 2009;44:431)
📌Parosteal osteosarcoma: most common surface osteosarcoma
📌Low grade central osteosarcoma: 1 - 2% of osteosarcoma
📌Periosteal osteosarcoma: rare (less common than parosteal osteosarcoma).
📌High grade surface osteosarcoma: rare (< 1% of osteosarcoma)
📌Extraskeletal osteosarcoma: rare; usually occurs in adults
- Low grade central osteosarcoma
- Conventional osteosarcoma
- Osteoblastic
- Chondroblastic
- Fibroblastic
- Secondary
- Small cell osteosarcoma
- Telangiectatic osteosarcoma
- Parosteal osteosarcoma
- Periosteal osteosarcoma
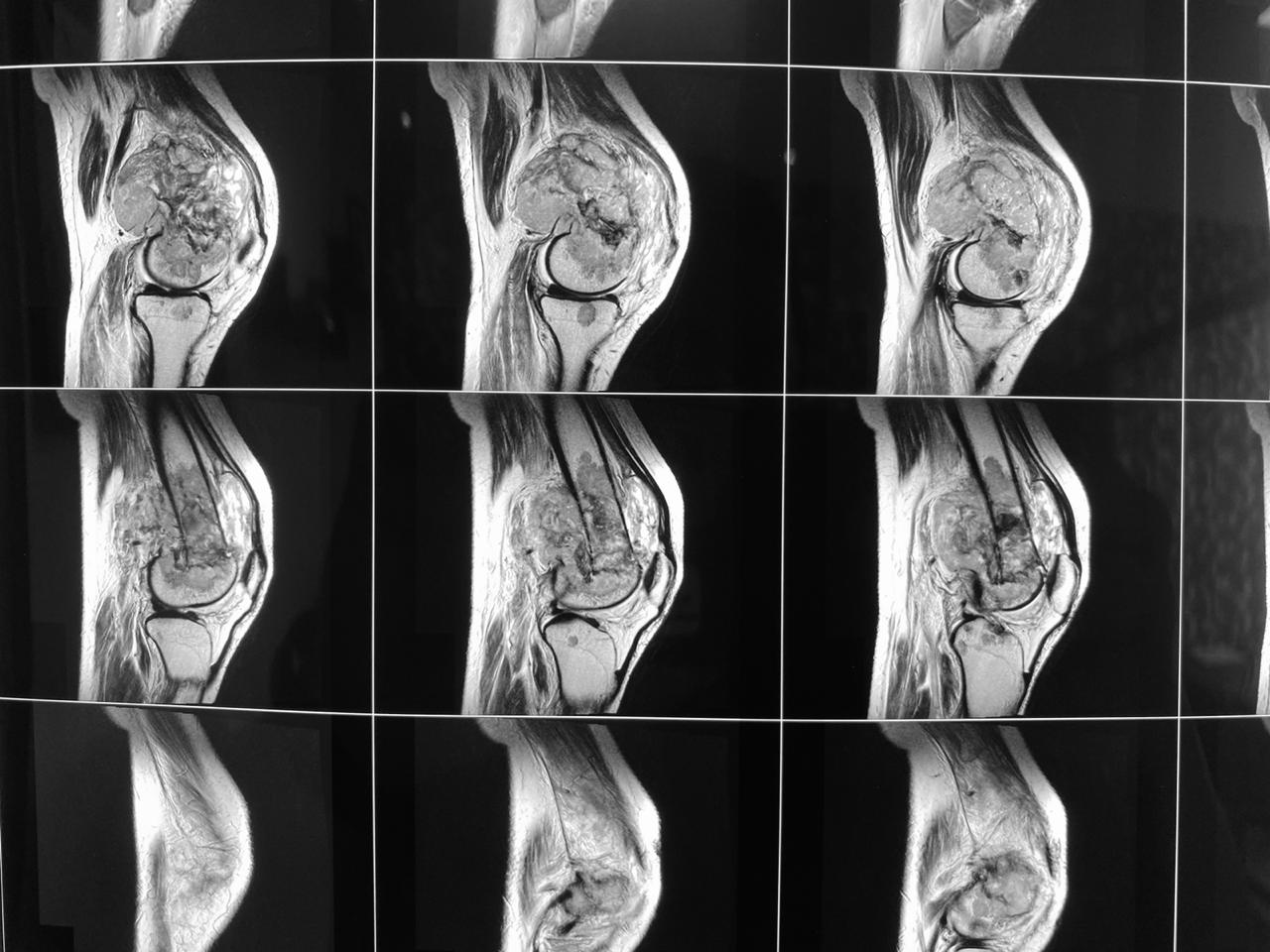
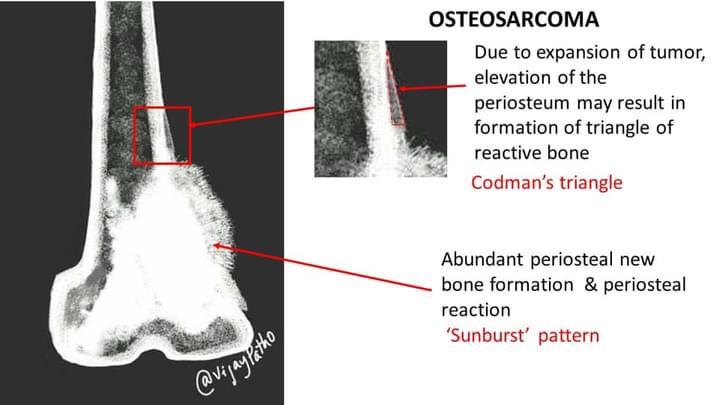
Radiology description:
📍 Invasive, destructive intraosseous mass (mixed lytic and blastic)
📍 Cortical permeation and soft tissue invasion common
📍Mineralization (often, most prominent centrally)
📍Periosteal reactions: Sunburst pattern or
Codman triangle: tumor permeates cortex and lifts up periosteum, then bone is deposited in periosteum creating a triangle.
 Codman triangle: tumor permeates cortex and lifts up periosteum, then bone is deposited in periosteum creating a triangle.
Codman triangle: tumor permeates cortex and lifts up periosteum, then bone is deposited in periosteum creating a triangle.
Sunburst periosteal reaction reflects aggressive periostitis. The sunburst appearance occurs when the lesion grows too fast and the periosteum does not have enough time to lay down a new layer and instead the Sharpey's fibers stretch out perpendicular to the bone. It is frequently associated with osteosarcoma but can also occur with other aggressive bony lesions such as an Ewing sarcoma or osteoblastic metastases (e.g. prostate, lung or breast cancer). Case courtesy of Dr Aditya Shetty, Radiopaedia.org, rID: 27260
- 📚 Conventional (high grade) osteosarcoma:
- Aggressive local growth and early hematogenous dissemination (lung metastasis, skeletal metastases)
- Nonmetastatic disease: 60 - 70% 3 year event free survival with current treatment (neoadjuvant chemotherapy followed by resection) (Acta Orthop 2011;82:211)
- Poor prognostic factors:
- Metastatic tumor (lung, skeletal, pleura, heart) (J Clin Oncol 2002;20:776)
- Axial tumor site (opposed to extremities)
- Status post neoadjuvant chemotherapy: (Cancer 1993;72:3227; J Clin Oncol 1988;6:329)
- Prognostic relevance most significant in the absence of metastatic disease
- Good prognosis: grades III / IV (significantly improved overall and recurrence free survival at 5 and 10 years)
- Poor prognosis: grades I / II (significantly reduced overall and recurrence free survival at 5 and 10 years)
📚 Parosteal and low grade central osteosarcoma:
- 5 year overall survival: ≥ 90% (Clin Orthop Relat Res 2008;466:1318)
- Dedifferentiation (~15 - 25% of cases): poor prognosis (similar to conventional high grade osteosarcoma) (Clin Orthop Relat Res 2008;466:1318)
📚 Periosteal osteosarcoma:
- 5 year overall survival: ~ 89%
- 10 year overall survival: ~ 83% (Clin Orthop Relat Res 2006;453:314)
- Metastasis: ~ 15%
📚 High grade surface osteosarcoma: prognosis is similar to conventional (high grade, intramedullary) osteosarcoma
📚 Extraskeletal osteosarcoma:
- 5 year overall survival: ~ 25%
Gross description:
✅Conventional (high grade intramedullary) osteosarcoma: Intramedullary mass: usually a metaphyseal epicenter (90%) with cortical permeation and a soft tissue component that raises the periosteu of long bones. Size (mean): 5 - 10 cm, cut surface: gritty and mineralized (hard) - may have cartilaginous areas (chondroblastic osteosarcoma), hemorrhage, necrosis and cystic change.
✅Parosteal osteosarcoma: Hard lobulated mass: attached to cortex, variable: nodules of cartilage partially capping tumor surface, variable dedifferentiated soft fleshy areas.
✅Low grade central osteosarcoma: Often fills entire metaphysis and diaphysis of involved bone.Firm, gritty cut surface, may demonstrate cortical destruction, periosteal reaction and soft tissue invasion.
✅Periosteal osteosarcoma: Broad based (sessile) tumor arising from the cortical surface (may circumferentially involve bone), cortex is thickened with scalloping of external surface. Heavily ossified base of tumor. External aspect of tumor (often the majority of the tumor) is cartilaginou. Calcified spicules may extend perpendicularly from the cortex within the mass and intermix with the cartilage. Rare to see cortical permeation and medullary extension.
✅High grade surface osteosarcoma: Tumor arises from the cortical surface and erodes / invades the corte,cut surface may be osteoblastic, chondroblastic or fibroblastic; areas of necrosis present. Status post neoadjuvant chemotherapy: To gross: cut along long axis of tumor and map.
Histopathology of osteosarcoma 📚 :
- 📚Conventional (high grade intramedullary) osteosarcoma:
- Permeative growth: intramedullary permeative growth (replacement of medullary space, surrounds and erodes native trabeculae, fills Haversian systems) and cortical destruction with soft tissue invasion
- Neoplastic cells: marked atypia (pleomorphic, hyperchromatic)
- Multiple cell morphologies often present in one tumor (epithelioid, plasmacytoid, spindled, small round cells, clear cells, giant tumor cells)
- Neoplastic bone (necessary for diagnosis): no minimum quantity necessary
- Most common: filigree / lace-like disorganized woven bone (intimately associated with neoplastic cells)
- Broad sheets of bone
- Normalization: decreased cytologic atypia of neoplastic cells entrapped in the bone matrix
- Scaffolding (appositional neoplastic osteoid deposition): deposition of neoplastic osteoid on native trabeculae
- Nonneoplastic giant cells: ~ 25% of cases.
-

-
- 📚Histologic subtypes of conventional osteosarcoma: no prognostic significance
- Osteoblastic, chondroblastic and fibroblastic are based on the prominent matrix they secrete (often admixed in one tumor)
- Osteoblastic osteosarcoma: the predominant matrix is neoplastic bone (as described above)
- Chondroblastic osteosarcoma: the predominant matrix is high grade cartilage (never has low grade cartilage)
- Fibroblastic osteosarcoma: spindled to epithelioid cells, often with severe atypia, which may secrete extracellular collagen (may be extensive)
- Telangiectatic osteosarcoma: the tumor is multiloculated with large blood filled spaces; high grade malignant cells and neoplastic bone in septae (the imaging differential diagnosis is with aneurysmal bone cyst)
- Other morphologic variants: giant cell rich variant (numerous osteoclast-like giant cells), epithelioid variant, osteoblastoma-like variant, chondroblastoma-like variant, chondromyxoid fibroma-like osteosarcoma, clear cell variant, small cell varian.
RANDOM OSTEOSARCOMA CASES:
Convencional Osteosarcoma. courtesy Dr. Luis Soler. México.
Convencional Osteosarcoma, courtesy Dr. Luis Soler. México.
13 yo girl, proximal tibial mass. Convencional Osteosarcoma, biopsy, High Grade histology. courtesy: K. Greg Mayhall. USA.
- Osteoblastic, chondroblastic and fibroblastic are based on the prominent matrix they secrete (often admixed in one tumor)











































Comentarios
Publicar un comentario